Bridging the Gap by Building Collaborations

By Lyandysha (Lana) Zholudeva
As an undergraduate from a small liberal arts college that allowed me to explore three different career paths simultaneously, I searched for a graduate program that would have the same collaborative and supportive environment. Much like my undergraduate campus, Drexel offered the potential for exploring different areas of neuroscience research and different career paths. During the interview day, I remember meeting with graduate students who spoke of their interests in working as scientists within the government as well as in industry, alluding to faculty members who could counsel on those career options. As an undergraduate, I knew that this type of support and freedom for a student would be crucial to my success in graduate school.
Capitalizing on Drexel's collaborative environment, I decided to build my thesis work on a collaborative project I had initiated between Drs. Itzhak Fischer (visit lab) and Michael Lane (visit lab). As part of Dr. Fischer's laboratory, I was able to master the methods necessary for culturing neural progenitor cells (NPCs) and for testing the therapeutic potential of grafting neuronal and glial restricted progenitors into the injured spinal cord of adult rats. As part of Dr. Lane's laboratory, I utilized my knowledge of NPCs to test whether transplantation of these cells can promote repair of a specific motor circuit that controls breathing. My findings have been well received by mentors and colleagues, sparking new and fruitful collaborations, and raising challenging questions for the field of cell transplantation.
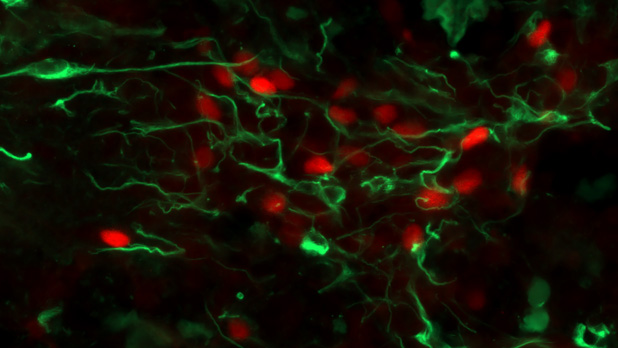
A confocal image showing developing rat spinal cord-derived tissue (embryonic day 13.5) 3 days after it has been transplanted into an injured adult rat spinal cord. The injury in this case was a cervical level spinal contusion. This transplanted tissue is rich with developing spinal interneurons (SpINs), which have been shown to be key cellular elements for neuroplasticity after injury. One particular subtype – the V2a SpINs - is immunohistochemically labeled with a transcriptional factor Chx10 (red), while nestin (green) stains immature neural tissue. These cells have been shown to play an important role in neuroplasticity of both respiratory and locomotor circuits after injury or disease and may represent an important therapeutic target. Cover image for Journal of Neuroscience Research. December 2018: Zholudeva and Lane (2018).
One of these collaborations is with Dr. Shelly Sakiyama-Elbert, chair of the Biomedical Engineering Department at the University of Texas, Austin, whose research team has successfully engineered a cell-line of excitatory interneurons (the V2a class) that I have been using to enrich our NPC transplants. Our decision to test the V2a interneurons emerged from yet another collaborative project in our department between our lab and the lab of Dr. Kim Dougherty (visit lab), a world-renowned expert on these interneurons. Our study revealed that spinal V2a interneurons become recruited into phrenic (respiratory) networks after injury.
Building upon these findings, the second part of my thesis work assessed the therapeutic efficacy of these V2a cells transplanted into a contusion spinal cord injury, using a comprehensive battery of molecular, anatomical, behavioral and electrophysiological outcome measures. Our findings demonstrated that enriched V2a-NPC transplants were most effective at enhancing respiratory plasticity after injury, compared to either NPC or vehicle controls. This project brought together four separate laboratories to test an innovative transplantation strategy for repair of the injured central nervous system.
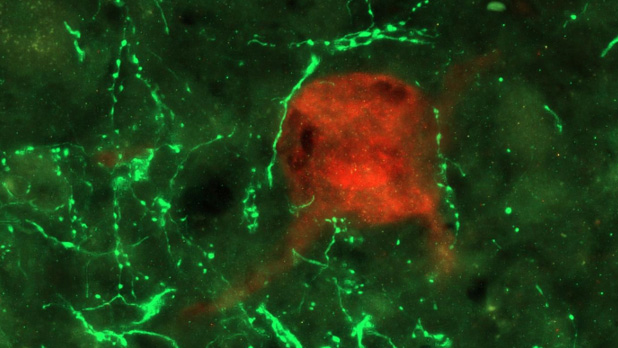
Pseudorabies virus (PRV) positive, phrenic interneuron (red) part of the host spinal phrenic circuit surrounded by green fluorescent protein positive (GFP, green) donor neural progenitor cells (NPCs) after transplantation into the injury site of a spinal cord. This image was taken one month after transplantation into a one-week old cervical contusion spinal cord injury.
I am extremely grateful for the collaborative environment that resulted in several publications and awards, indicators not only of a student's success, but also of the mentors and institution. Besides the opportunities for excelling in academics, what I value the most about Drexel and the Neurobiology department is how students are perceived not as mere trainees but as fellow scientists with valid thoughts and ideas. In part, this is due to the mentors Drexel has provided me with, including my advisor, Dr. Lane, who placed high importance on my personal and professional growth, not only advising on my research but also facilitating my networking in the field.
The new relationships I gained in the process have yielded fruitful collaborations, future employment opportunities and, perhaps even more importantly, lifelong friendships. I am grateful for the skills and values that Drexel has contributed in my training as a graduate student and I am confident they will help me become an effective researcher and a mentor to my own students someday.
Back to Top