January 24, 2024
By Tara Lamb, Drexel University College of Medicine
For far too long disparities in the health care system, whether it was race, socioeconomic class or gender identity, have had a major impact on patients. Today we still see disproportionate measures when it comes to cancer and how it is diagnosed and treated. Breast cancer is the most common non-cutaneous cancer, with hundreds of thousands of new cases each year. Due to the increase in early detection and more effective treatments, the overall mortality rate due to breast cancer has decreased over the years1. However, the mortality rate remains higher in Black women than white women2. There are several factors that are thought to contribute to this discrepancy, one of them being the differences in the treatment of breast cancer between these groups. Black women, when compared to white women with the same stage of disease, are less likely to receive a timely diagnosis and are often not given the same recommendations of treatment options3. Post treatment there is an inconsistency again with physician recommendations and the options that are given to patients regarding breast reconstruction. Connors et al. decided to further investigate why there is a disparity in breast reconstruction after a mastectomy. They noticed that Black women had a significantly lower reconstruction rate and significantly higher rate of autologous breast reconstruction as opposed to implant reconstruction. They also found that Black women had significantly larger proportions of public health insurance, aggressive tumors, unilateral mastectomies and modified radical mastectomies4.
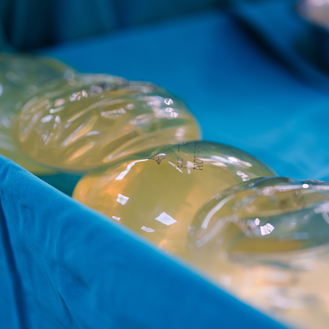
As mentioned above, there are several breast reconstructive options available to women including autologous (tissue), implant-based or a combination of both. Each method has its own risk and benefit profiles and should be considered on a patient-to-patient basis5. Autologous breast reconstruction can be done in cases after a mastectomy or after radiation therapy when there is insufficient tissue left on the chest wall to cover and support a breast implant, or in some cases patients may choose not to have an implant procedure for personal reasons. Autologous breast reconstruction can be further classified into different subtypes based on the composition of the flap or source of the tissue and blood supply6. A flap in surgery is a technique used when lifting any type of tissue from a donor site and moving it to a recipient site with intact blood supply7. Some of the more common sources/locations for flaps are the back and the abdomen for a breast reconstructive procedure6.
While there are a variety of techniques available to perform breast reconstruction post mastectomy, it is very important to consider the risk and benefit profiles of the procedure, and individualize each procedure specific to the patient. There are several complications that can occur during and after a procedure and some procedures are more prone to specific complications than others. There are several ways to categorize complications. Some local complications that can occur are total/partial flap loss and necrosis, skin necrosis, seromas, bleeding or hematomas. Complications that can occur after an implant procedure include but are not limited to capsular contracture around the implant, capsular fibrosis, implant rupture, wrinkling and palpability, and breast asymmetry5.
There are also several other factors that can have an influence on the outcome of these procedures and affect the overall healing process. Some of these factors include current smoking, diabetes, older age and a higher BMI5,8,9. Patient populations that come from a lower socioeconomic class and are considered Black regarding race tend to have poorer health outcomes. While there has been great work done to bridge the gap among different patient populations across the board in health care, there is still a way to go.
Sources/Resources:
- World Health Organization. Breast cancer facts. Retrieved from https://www.who.int/cancer/prevention/diagnosis-screening/breast-cancer/en. 2004
- Wheeler SB, Reeder-Hayes KE, Carey LA. Disparities in breast cancer treatment and outcomes: biological, social, and health system determinants and opportunities for research. Oncologist. 2013;18(9):986-93. doi: 10.1634/theoncologist.2013-0243. Epub 2013 Aug 12. PMID: 23939284; PMCID: PMC3780646
- Yedjou CG, Sims JN, Miele L, Noubissi F, Lowe L, Fonseca DD, Alo RA, Payton M, Tchounwou PB. Health and Racial Disparity in Breast Cancer. Adv Exp Med Biol. 2019;1152:31-49. doi: 10.1007/978-3-030-20301-6_3. PMID: 31456178; PMCID: PMC6941147
- Connors SK, Goodman MS, Myckatyn T, Margenthaler J, Gehlert S. Racial Disparities in Breast Reconstruction at a Comprehensive Cancer Center. J Racial Ethn Health Disparities. 2021 Oct 13. doi: 10.1007/s40615-021-01169-3. Epub ahead of print. PMID: 34647274
- Wilkins, E. G. , Hamill, J. B. , Kim, H. M. , Kim, J. Y. , Greco, R. J. , Qi, J. & Pusic, A. L. (2018). Complications in Postmastectomy Breast Reconstruction. Annals of Surgery, 267 (1), 164-170. doi: 10.1097/SLA.0000000000002033
- Brumby, Daisy and Gabby Shacknai. “Breast Reconstruction Options.” American Society of Plastic Surgeons, https://www.plasticsurgery.org/reconstructive-procedures/breast-reconstruction/techniques
- “Breast Reconstruction with Flap Surgery.” Mayo Clinic, Mayo Foundation for Medical Education and Research, 29 Dec. 2020, https://www.mayoclinic.org/tests-procedures/breast-reconstruction-flap/about/pac-20384937
- Bennett KG, Qi J, Kim HM, Hamill JB, Pusic AL, Wilkins EG. Comparison of 2-Year Complication Rates Among Common Techniques for Postmastectomy Breast Reconstruction. JAMA Surg. 2018;153(10):901–908. doi:10.1001/jamasurg.2018.1687
- Mak JC, Kwong A. Complications in Post-mastectomy Immediate Breast Reconstruction: A Ten-year Analysis of Outcomes. Clin Breast Cancer. 2020 Oct;20(5):402-407. doi: 10.1016/j.clbc.2019.12.002. Epub 2020 May 23. PMID: 32665188