Telemedicine:
Changing the Face of Health Care
By Nancy West
Even before the COVID-19 pandemic changed the world as we know it, telemedicine was on the verge of transforming health care. The global telemedicine market was projected to reach $19.5 billion by 2025, a 225 percent increase from $6 billion in 2016, according to a 2018 research study by Transparency Market Research. IHS Markit estimated that telemedicine visits in the United States would soar from 23 million in 2017 to 105 million by 2022. Now those projections could increase exponentially, fueled by the safety considerations and social distancing required to fight COVID-19.
What exactly is telemedicine? The Department of Health and Human Services defines it as "the use of electronic information and telecommunication technologies to support and promote long-distance clinical healthcare, patient and professional health-related education, public health and health administration." Telemedicine can be conducted via video visits, telephone visits, electronic messaging, virtual consults and remote patient monitoring with digital technology.
What is fueling its rapid growth? Besides the current COVID-19 pandemic, many factors are involved. Patients want convenience and an easy way to connect with their health care providers. At the same time, federal and state regulatory changes going into effect will reduce or eliminate longstanding financial barriers as more insurance companies begin to cover telemedicine visits. By the end of last year, 40 states and the District of Columbia had private payer laws in effect. Also, in 2019, the Centers for Medicare and Medicaid Services approved reimbursement for three services:
- Virtual check-ins, when the health care provider has a brief remote check-in with an established patient to assess whether an office visit is needed.
- Remote evaluation of recorded video, images and other patient-generated information to evaluate a patient's condition.
- Interprofessional internet consultations performed for the benefit of the patient.
On March 6, 2020, in response to the COVID-19 pandemic, CMS expanded the telemedicine benefit to include office, hospital and other visits provided via tele medicine across the country, including a patient's places of residence, with the 1135 waiver authority and Coronavirus Preparedness and Response Supplemental Appropriations Act. Physicians, nurse practitioners, clinical psychologists and licensed clinical social workers are now able to offer telemedicine to their patients. Government experts anticipate that daily visit volumes for telemedicine providers will increase from 50,000 to 100,000 industrywide during the pandemic. Some experts expect CMS to continue this expansion of benefits after the COVID-19 crisis has passed.
Advanced technology has also stimulated the growth of telemedicine by enhancing its efficiency and effectiveness. The quality of telemedicine consults has been demonstrated in many studies (by the Veterans Health Administration and the Agency for Healthcare Research and Quality, among others). And insurers and patients are realizing significant cost savings.
Back to the Future

Telemedicine is not a 21st-century development. Its roots are in the 1960s and '70s, most notably when the National Aeronautics and Space Administration wanted to ensure that an advanced program for remote monitoring could lead to stronger medical support for astronauts during long-duration space missions. To test the advanced system, NASA created an earthbound analog, partnering with the Indian Health Service and the Papago people (now the Tohono O'odham Nation) of southern Arizona in a project called STARPAHC [Space Technology Applied to Rural Papago Advanced Health Care], which provided Native Americans on the remote Papago Reservation with access to physicians at Indian Health Service hospitals. NASA used microwave technology to transmit X-rays, electrocardiographs and other medical information. Projects like this stimulated research in the field of medical engineering, which in turn led to rapid growth for telemedicine.
One College of Medicine alumnus, retired Army Col. Ron Poropatich, MD, HU '85, pioneered the use of telemedicine in the U.S. military, starting in 1992 when the Army deployed troops to Somalia for a humanitarian peacekeeping mission. Army officials wanted to have remote consultation capability to ensure that the troops got the best care.
"We figured out a simple system to send information back to Walter Reed Army Medical Center so physicians could review dermatology and infectious disease cases," says Poropatich, who is the director of the Center for Military Medicine Research at the University of Pittsburgh, as well as a professor of medicine in the Division of Pulmonary, Allergy, and Critical Care Medicine. "1992 was a breakthrough year for digital photography, so we took a Kodak digital 1.54-megapixel camera — for perspective, the average cell phone today has 10 megapixels or greater — and an Apple MacIntosh laptop computer. I downloaded digital images from the camera to the laptop and sent them to Walter Reed via the International Maritime Satellite system."
This simple system gained great acclaim, and in the ensuing years, Poropatich oversaw the implementation of telemedicine capabilities in more than 80 sites each in Afghanistan and Iraq, as well as locations in Croatia, Macedonia, Kenya and Haiti. In 1995, he developed and implemented telemedicine capabilities back home to meet the needs of active duty military and retirees for the 21-state North Atlantic Regional Medical Command.
Telepsychiatry
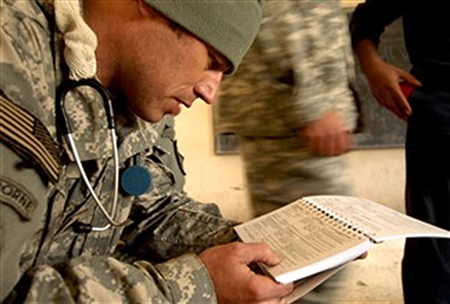
"In 1995, we could stand up a large behavioral health program with telepsychiatry consults both stateside and overseas," notes Poropatich. "In combat zones, it was challenging because we had people shooting at us, we were dealing with dust storms, and troops were scattered over large geographic spaces. We always want to provide the best possible care to isolated, small military bases like a command outpost or forward operating base. Those regions have concentrations of soldiers with medical needs. They can't just get in the car and drive to the nearest doctor.
"We were able to provide video consults at these outposts so the troops could see the provider face to face," he continues. "We try to fly providers in for in-person consults, but flights are often grounded due to weather or military conflict. Instead of stopping the psychiatry consult, the provider is still able to see patients via telemedicine. This is so important because these young men and women deal with so much stress. They often need professionals to help them cope, and telemedicine allows us to do that. It worked well in 1995 and continues to work well."
During his military career, Poropatich served as telemedicine and medical informatics consultant for the Army from 2000 to 2008 and as deputy director for the Telemedicine & Advanced Technology Research Center. He also ran telemedicine for NATO from 2000 to 2012, which involved standardizing telemedicine across all military forces in 26 member nations.
In 2008, Poropatich implemented mCare, a secure mobile messaging program that provides mobile health to wounded warriors using their existing cell phones. In 2010, it was voted the Army's greatest invention.
Today the Army's telemedicine program has doctors in 25 different specialties who put information in "store-and-forward" — an electronic transmission of prerecorded videos, medical records and digital images — so that anyone can ask a question and get an answer within one or two hours anywhere in the world.
Tele-benefits

In the civilian world, Steven V. Gurland, MD, HU '67, also played a key role in the growth of telemedicine. After a career first as an internal medicine specialist and then medical director for a managed care company, Gurland was looking for a new challenge. He saw telemedicine as the future and invested, along with his partner, in the technology to support it. In 2009, they co-founded MDLive, a virtual health care services company with a network of board-certified physicians, dermatologists, psychiatrists and therapists.
Employers and third-party administrators contract with MDLive to provide telemedicine benefits for employees.
"To me, it was an obvious service that was needed," says Gurland. "We could provide access to care at a very low cost, which was what our health care system was crying for. It was a matter of convincing patients that it was a good way of communicating and, more importantly, convincing physicians and payors that it was something of value."
Even before COVID-19 struck, MDLive was thriving, with more than 30 million patient members nationwide.
"We have grown tremendously because we've proven over the years that the more patients who are treated through telemedicine, the more money the payor saves. We definitely decrease the number of unnecessary ER visits and urgent care visits," Gurland says. "Our members love it because, within 10 minutes, you can speak to a board-certified physician, and that is of immeasurable value. They think it's fantastic because they don't have to wait in a sick waiting room, or go to an urgent care center, or spend thousands of dollars for something that's relatively simple to take care of."
MDLive recently began offering primary care services enabled by new technology. "You can truly examine a patient at home through the computer. You can listen to their heart and look in their throat and ears. Technology has gotten so much more affordable than when we first started. The remote monitoring equipment used to cost $5,000. Now you can get the same technology for $200. It makes sense for the insurance company to pay for the patient to receive this care at home so they don't have to visit the ER or the doctor," notes Gurland.
In response to the COVID-19 pandemic, MDLive announced initiatives to prepare for a significant expansion of services. As of March 19, the company reported a greater than 50 percent increase in utilization of its virtual platform since the start of the outbreak in the United States.
What Lies Ahead?
Most immediately, telemedicine will play a critical role in caring for patients with COVID-19.
"Eighty percent of COVID-19 cases are mild to moderate, not requiring hospitalization," says Poropatich. "Fifteen percent are severe, requiring hospitalization and supplemental oxygen. Five percent are critical, with patients admitted to the ICU on mechanical ventilators. The vast majority of patients in the 80 percent mild-to-moderate category can receive care through telemedicine.
"Enabling patients to receive care at home with remote monitoring technology connected to the whole telemedicine health care team is going to be really important in fighting COVID-19," he continues. "I think more and more people will be going online and buying a pulse oximeter, blood pressure monitor and other simple technology to have at home. Having these and other vital sign readings will enhance our ability to provide effective care via telemedicine."
In the current environment, people with chronic diseases and other health problems don't want to venture from home because of the risk of exposure to COVID-19. "We already do a lot of monitoring of patients with chronic disease," Poropatich says. "At the University of Pittsburgh Medical Center, we have diagnostic kits that we lend to people with COPD, asthma, congestive heart failure and severe diabetes, among other conditions," he adds. "Telemedicine enables them to get the care they need without unnecessary risk of exposure."
Lawrence Fried, MD '11, a pediatric neurologist at Children's Hospital of Philadelphia who specializes in epilepsy, is using telemedicine to continue care for his patients while keeping everyone safe during the COVID-19 pandemic. "The technology that we are using is embedded within our electronic medical record system, and is very easy to use," he says. "My patients all seem to love our virtual visits. They are more comfortable at home, and it's less stressful for them than having to come into the city, especially during these times."
Generally speaking, Fried finds telemedicine most effective for follow-up visits with patients. "For initial encounters, an in-person visit is still preferable because the physical exam is such an important component. You can't test reflexes via phone or computer," he notes. Over the long haul, he believes telemedicine visits offered alternately with office visits would be very effective (see below).
Pretty soon, according to Gurland, "very few conditions will require patients to go to the office. Most things — both acute illnesses and chronic — will be taken care of through telemedicine at home. All primary care will be done that way. With the new payment methods, you're going to see a tremendous amount of specialty work using telemedicine."
Poropatich says, "Cell phones are going to be the way to go in the future. Smartphone apps will probably morph into artificial intelligence in health care. You're going to use your cell phone to take a picture that will tell you what your rash is.
"To me, telemedicine augments care," he continues. "It's really hard to replace face-to-face visits entirely. But the technologies we have are going to make health care providers better at what they do by packaging the patient's medical information in a way that saves time. All this information is going to be on a cell phone. The cell phone is going to be the key tool for educating patients about how to lead a better and healthier life."
Telemedicine for a Warm Transfer
Pediatric neurologist Lawrence Fried, MD '11, is the co-principal investigator for a grant from the Health Resources and Services Administration to study transition of care as pediatric epilepsy patients age out, to study the use of telehealth and telemedicine strategies, and to strengthen relationships between primary care physicians and pediatric epileptologists at Children's Hospital of Philadelphia.
The team's research into telemedicine includes establishing a telemedicine clinic with a special focus on easing the transition of teenage patients from their pediatric neurologist to an adult neurologist.
"There's a lot of fear on the part of the families facing this transition because a lot of these kids have been seeing their pediatric neurologist almost their whole lives," Fried notes. "This longstanding relationship is now ending, and that's always scary.
"We are using a video interface with the pediatric provider, the patient and their family on one end and, on the other end, a nurse practitioner and physician team to help facilitate the transfer of care from pediatric to adult — a warm transfer. This helps to give the family a familiar face to look for when they make the transition. The video visits are more than just a meet and greet. It's also a brief review of the medical record and the psychosocial situation as well.
"We hope to expand the use of telemedicine to actually supplement in-person office visits with telemedicine visits, to reduce disruptions for patients who have geographic barriers and to facilitate access to care. This may also improve physician satisfaction, potentially reducing burnout, which has been widely reported in the profession."
Back to Top