A Classic Pulmonary Embolism
By: Michael Murray, DO
69 year-old African American male with past medical history of diabetes mellitus type II and hyperlipidemia presents after experiencing acute shortness of breath while walking across a parking lot after grocery shopping, followed by near syncopal episode which he describes as "my body gave out." He denies loss of consciousness, and immediately called 911.
On arrival to the emergency department he was in moderate to severe respiratory distress saturating 85% on 3L NC. The remainder of his vitals were as follows; temperature 97.5 F, heart rate 125 (normal sinus rhythm on the monitor), respiratory rate 22 and blood pressure 117/90.
The patient was placed on non-rebreather with improvement of his saturations to the mid 90's. On initial evaluation the patient looked to be in moderate to severe distress. His heart exam was tachycardic but without murmur. His lungs were clear to auscultation bilaterally. There were no signs of peripheral edema.
Bedside point of care ultrasound (POCUS) was preformed to further evaluate heart and lungs. Using the phased-array probe lungs were evaluated for lung sliding and B lines. The patient was found to have appropriate lung sliding with no indication of pneumothorax and no B lines which would indicate pulmonary edema. Echocardiogram showed a dramatically dilated right ventricle (RV) with poor RV function in the parasternal long view.
Parasternal short view further demonstrated dilated right ventricle with "D" sign (septal flattening)
Simultaneously electrocardiogram was obtained demonstrating an S1Q3T3, anterior/septal T wave inversions with depressions in V2-V4.

Based on POCUS findings and EKG demonstrating right heart strain the patient was sent directly to CT angiography of his chest, prior to obtaining laboratory results.
CTA showed filling defects within all major lobar branches of the pulmonary arteries (submassive pulmonary embolism), with enlargement of the right ventricle and flattening of the interventricular septum (right heart strain).
The patient was started on a heparin drip in the emergency department and with medical ICU consultation the decision was made to send him directly to interventional radiology for catheter directed tPA rather than systemic thrombolytics.
Following admission and catheter directed tPA, ultrasound of the lower extremities were obtained and showed acute non occlusive DVT in the left popliteal vein.
Teaching Points
Systemic vs catheter directed thrombolysis:
Systemic fibrinolysis has been shown to quickly and effectively decrease thrombus burden and pulmonary artery pressures resulting in clinical improvement however there is a risk of major bleeding including intracranial hemorrhage. Given this risk pulmonary embolism patients generally only receive systemic thrombolysis in significant hemodynamic compromise or cardiogenic shock. Catheter directed thrombolysis (tPA) is becoming increasingly more utilized as it results with reduced thrombolytic dose and as a result less major bleeding risk. This decision is typically made in conjunction with interventional radiology and with the ICU.
POCUS in acute PE:
Generally we are looking for signs of elevated pulmonary artery pressures and right heart strain. These findings can be demonstrated by RV wall hypokinesis, RV dilation, RA dilation, paradoxical septal systolic motion and dilated IVC with lack of respiratory collapse. There were two classic ECHO findings in our case.
"D" sign in parasternal short view:
In a physiologically normal heart the left ventricular pressure is greater than the right ventricular pressure. Therefore when viewing the heart in a parasternal short axis (cross-sectional view of both right and left ventricles) during systole the left ventricle maintains a circular appearance, bowing the intraventricular septum into the right ventricle as shown below (image taken from emergencyultrasoundteaching.com).

Aptly named for the shape the LV takes when the RV is dilated and produces paradoxical septal wall motion the "D" sign is found in the parasternal short axis with increased pulmonary artery pressures and RV strain which you can see below, first in the labeled still shot and second as we saw live in the department. Please also notice the dramatically dilated right ventricle which further indicated right heart strain and increased right sided pressures.
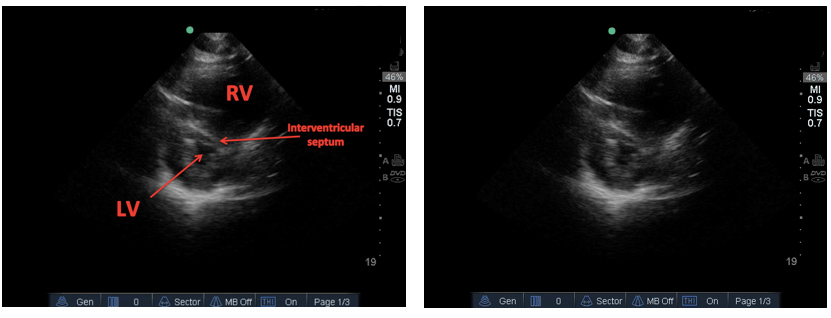
McConnell's sign:
In a physiologically normal heart there should be concentric and symmetrical contraction of both ventricles. McConnell's sign is an echocardiographic finding demonstrating hypokinesis of the superior and mid right venticular free wall with preservation of apical wall function. Typically McConnell's sign is demonstrated in the four chamber view. In our case we were unable to obtain a four chamber view however, in the parasternal long view right ventricular hypokinesis is demonstrated in addition to RV dilation. Like above first is a labeled image still shot and then the live version we saw in the department finally followed by a classic McConnell's sign taken from 5 Minute Sono Blog.
Please see "IS MCCONNELL’S SIGN USEFUL FOR APE?"
EKG in PE:
Admittedly EKG is not the optimal test in evaluating for pulmonary embolism however there are definitely classic findings which can raise suspicion in obtaining more definitive testing. Like in ultrasound these are findings suggestive of right heart strain, elevated pulmonary artery pressures and RV dilation.
- S1Q3T3 – The most classic and tested EKG finding in PE. It is found in approximately 20% of PE's depending on what source you look at.
- T wave inversion in right precordial and inferior leads – Simultaneous T wave inversions in the inferior and right precordial leads is the most specific finding in favor of PE, with reported specificities of up to 99% in one study. (Kosuge et al)
- Clockwise rotation - shift of the R/S transition point towards V6 with a persistent S wave in V6 implies rotation of the heart due to right ventricular dilatation
- Dominant R wave in V1
- New right axis
Shown below is the EKG obtained in our case, which you can see has S1Q3T3, simultaneous T wave inversions in inferior and right precordial leads and ST segment depression.

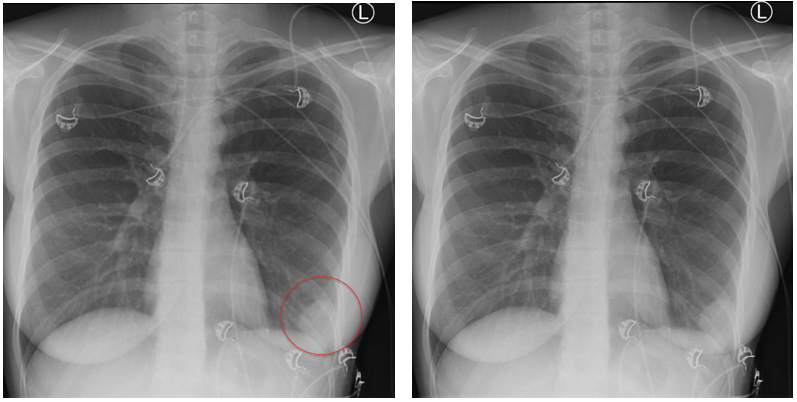
Though not evident in our case there are two classically tested chest x-ray findings in PE.
Westermark Sign: a decrease in vascular markings in the area distal to the pulmonary embolism. The physiologic theory is pulmonary artery occlusion vs. distal vasoconstriction in hypoxic lung. The following images are taken from radiopaedia.org.
Courtesy of Dr. Mike Murray
Keywords: pulmonary embolism, Westermark sign, S1Q3T3

Hampton's Hump: a wedge shaped opacity in the lung field, often at the lung base representing lung infarction distal to the vascular occlusion. Again images taken from radiopaedia.com.
The information on these pages is provided for general information only and should not be used for diagnosis or treatment, or as a substitute for consultation with a physician or health care professional. If you have specific questions or concerns about your health, you should consult your health care professional.
The images being used are for illustrative purposes only; any person depicted is a model.
Back to Top