Emergency Medicine Teaching Case: A Case of Myopericarditis
HPI:
21yo male with no past medical history presents to the ED complaining of intermittent chest pain x 1 day. Chest pain is substernal, pressure-like without radiation or modifying factors. He denies any associated palpitations, orthopnea, or lower extremity edema. Otherwise, no fever, chills, diaphoresis, sweats. No coughing, dyspnea, hemoptysis, or wheezing. No nausea or vomiting. Denies family history of significant cardiac disease. Denies PE/DVT risk factors. No heavy lifting or recent trauma.
Of note, patient states that he had URI symptoms that started 5 days prior to the onset of symptoms. States that he had rhinorrhea and a non-productive cough that resolved in 3 days.
Exam:
VS: BP 127/83, HR 61, RR 18, SpO2: 99% on room air, T 97.9F.
General: AAOx3, well appearing, NAD.
HEENT: Normocephalic, atraumatic. PERRL, EOMI. Oropharynx clear without posterior pharyngeal erythema or exudates.
Neck: No JVD. Supple. No cervical lymphadenopathy.
Cardiovascular: RRR with S1 and S2. No murmur, rubs, or gallops.
Respiratory: Lungs clear to auscultation bilaterally.
GI: Soft, non-distended, non-tender.
Extremities: No calf tenderness or edema. No clubbing, cyanosis.
Neuro: AAOx3, grossly non-focal.
Initial EKG obtained at triage:
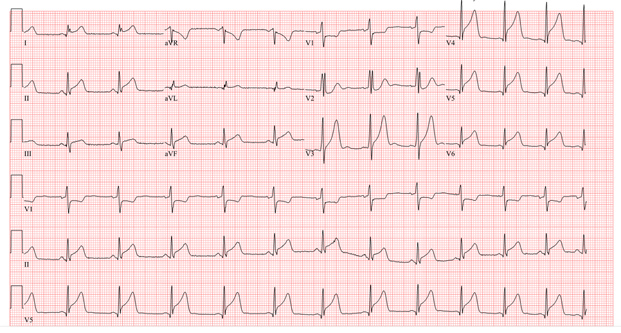
- Given that the initial EKG showed diffuse ST elevations with J point elevations, along with ST depressions in leads aVR and aVL, there was high concern for pericarditis.
- At the time of evaluation, the patient was well appearing without any pain at the time.
- While labs were pending, a bedside cardiac ultrasound was performed. Four views of the heart obtained including subxiphoid, parasternal long, parasternal short, and apical 4 chamber. There was no evidence of a pericardial effusion, wall motion abnormality, or right heart strain. The heart was noted to have adequate squeeze without an obviously depressed ejection fraction.
- Labs had returned with the following abnormalities:
- Troponin: 33.10 ng/ml (Normal range: < 0.04)
- CRP: 3.70 mg/dl (Normal range: < 0.30)
- ESR: 18 mm/hr (Normal range: 0-10)
- Otherwise, other labs (CBC, BMP, Rapid Influenza) and CXR were unremarkable.
- As soon as the troponin had returned from the lab, a call out to the cardiologist was made for further recommendations.
- The cardiologist recommended starting Aspirin 325mg daily and a bedside echocardiogram was performed in the ED.
- Echo was unremarkable.
- Ejection fraction was 57%
- No valvular pathology
- No pericardial effusion
- Patient was admitted for further work up and to trend EKGs and troponins.
- Over the next 3 days, the troponin had peaked to 39.9 before downtrending to 11.0 prior to discharge.
- Although there was a low concern for ACS, patient noted to have persistent, diffuse ST elevations on repeat EKGs.
- The patient had undergone a cardiac catheterization on the third day of admission prior to discharge with no evidence of coronary artery disease or coronary lesions.
- He was safely discharged after 3 days without any significant complications during his admission.

Courtesy of Dr. Kohtaroh Takamura, MD
Drexel University Emergency Medicine Residency
Class of 2019
Contact Information
Karima Sajadi-Ernazarova, MD
Associate Professor of Emergency Medicine
215.762.2374 | karimasajadi@gmail.com
The information on these pages is provided for general information only and should not be used for diagnosis or treatment, or as a substitute for consultation with a physician or health care professional. If you have specific questions or concerns about your health, you should consult your health care professional.
The images being used are for illustrative purposes only; any person depicted is a model.
Back to Top