Emergency Medicine Teaching Case: A Case of a Blue Hand
59 yo female with PMH DM/HTN/hypothyroidism and Reynauld’s phenomenon who presented to ED in the morning c/o increasing pain and paresthesia in right hand and it is turning blue since last night. Patient was at the outpatient phlebotomy site 1 day prior getting routing blood work done. Patient states she had multiple attempt at blood draw in her right decubitus fossa and right hand. Shortly after she came back home, she felt that her right hand started to be painful and swollen, then became colder to touch and finally started to turn blue. Patient called her MD who sent her to ED.
In triage, patient’s right hand looked like this:
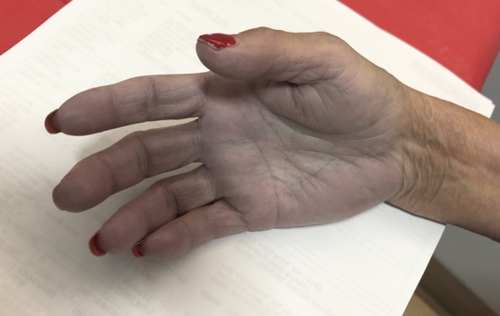
On exam, patient was in a moderate pain distress. Right hand was visibly blue and cold to touch. There were no ulnar or radial pulses by Doppler. Patient had pain to passive motion of the fingers. Cap refill was increased (see video):
After the initial exam, Vascular Surgery was notified and patient was taken to the IR. This is the angiogram of this patient, showing the segmental occlusion of the right proximal brachial artery measuring 4 cm in length:

Patient was taken to the OR for emergent thrombectomy and di well post-op.
Acute arterial occlusion:
- Acute occlusion of the artery equal limb ischemia and is a vascular emergency. Prompt diagnosis is a must!
- Definition: acute limb ischemia is a sudden loss of limb perfusion for up to 2 weeks after the initiating event. It can occur in any peripheral artery of upper or lower extremities.
- Acute arterial occlusion is time sensitive and if left undiagnosed/untreated can quickly progress to infarction and loss of limb and life. Acute arterial occlusion is associated with increased morbidity, significant disability, and emergent operation in high-risk patients.
- The most common cause of acute limb ischemia is in situ thrombotic occlusion. Other causes: embolic occlusion from the left heart, aorta, and iliac vessel, as well as penetrating or blunt trauma.
- The classic presentation of limb ischemia is known as the "six Ps": pallor, pain, paresthesia, paralysis, pulselessness, and poikilothermia.
- Cases of limb-threatening ischemia require emergent vascular surgery consult. The surgical approach is directed at reperfusion of the affected extremity. This can be accomplished by the surgical bypass, endarterectomy, or embolectomy. Results are variable and will ultimately depend on the duration of the ischemia and the extent of occlusion.
Teaching pearls:
- Your job as ED doc is to promptly recognize the acute limb ischemia and call stat vascular surgery consult.
- Do not waste time doing imaging!
- Have a high index of suspicion and know the signs of limb ischemia: pallor, pain, paresthesia, pulselessness, poikilothermia.
- Know risk factors: age, smoking, diabetes, obesity, sedentary lifestyle, family history of vascular disease, high cholesterol, and high blood pressure.
- Non-traumatic ischemia of the lower extremities is more common than the upper extremities and is more likely to result in limb loss.
Keywords: acute limb ischemia, vascular emergency, artery occlusion, thrombectomy
Courtesy of Dr. Karima Sajadi
Contact Information
Karima Sajadi-Ernazarova, MD
Associate Professor of Emergency Medicine
215.762.2374 | karimasajadi@gmail.com
The information on these pages is provided for general information only and should not be used for diagnosis or treatment, or as a substitute for consultation with a physician or health care professional. If you have specific questions or concerns about your health, you should consult your health care professional.
The images being used are for illustrative purposes only; any person depicted is a model.
Back to Top