Collaborative Research by Drexel, Cooper Medical Students Demonstrates Method to Reduce Opioid Use Disorder Stigma
March 1, 2022
By Lisa Ryan
Last month, medical students from Drexel University College of Medicine and Cooper Medical School of Rowan University published research that reduces negative stigma about people with opioid use disorder through overdose reversal training sessions.
Previous studies had established best practices for raising participants’ understanding of how to use naloxone to reverse an opioid overdose and building confidence in their ability to help someone during an overdose. Drexel and Cooper students were the first to demonstrate that their training sessions had a positive impact on participants’ view of people with opioid use disorder.
“In almost every instance, participants increased their desire to empathize and help people after the training,” said researcher Ben Haslund-Gourley, MD/PhD candidate, Class of 2026.

Ben Haslund-Gourley

Nick Bascou

Annette Gadegbeku, MD
Haslund-Gourley was one of several College of Medicine students who helped author the January 2022 paper. Other student researchers included Kyle Samson, MD/PhD Class of 2025, Nathaniel Goss, Dakota Meredith, Andrew Friedman, and Vishnu K. Kumar, all of the MD Program Class of 2023.
The students’ faculty advisor Annette Gadegbeku, MD, is an associate professor in the Department of Family, Community & Preventive Medicine and assistant dean of community health within the Office of Diversity, Equity & Inclusion, Drexel University College of Medicine
The paper is published in the Harm Reduction Journal as open access and is accessible to readers for free, thanks to funding support from Walter H. and Leonore Annenberg Dean, and Senior Vice President of Medical Affairs Charles B. Cairns, MD, FACEP, FAHA, and Drexel University’s Office of Research and Innovation.
Origins of the Study
The student researchers from the College of Medicine were all involved in the Naloxone Outreach Project (NOP), a student-run street medicine service provided in Kensington and other Philadelphia neighborhoods through the College of Medicine’s Health Outreach Project (HOP).
Students launched NOP in 2017 to help address the opioid epidemic by providing members of underserved communities with increased access to naloxone and a better understanding of how to use it to reverse an overdose.
In 2018, NOP created the Naloxone Outreach Interschool Collaborative (NOIC) to expand the NOP model to current students and alumni of Philadelphia-area medical schools. The NOIC enabled members of other medical school communities, including Cooper Medical School, to use NOP methods in their own street medicine outreach.
Haslund-Gourley said medical students are well-equipped to educate their peers and community members about opioid use disorder without bringing stigma to the table.
“Medical students are taught to understand the mechanisms of disease, while also keeping in mind these are human beings, not just statistics,” Haslund-Gourley said. “We can work with the community to shift their perspectives."
Nick Bascou, Cooper Medical School Class of 2022, was one of the Philadelphia-area medical students who took NOP’s overdose reversal training through NOIC and learned to train members of the Camden, NJ community with the same methods.
Bascou was already active by then in Cooper Medical School’s Street Medicine Outreach program, which provides personal care items, basic medical care, Narcan, and connections to primary care and substance use disorder treatment to Camden residents who are dealing with homelessness and opioid use disorder.
Bascou and Haslund-Gourley connected in 2021 to combine research by NOP and data from Bascou’s time with Street Medicine Outreach for what would become the January 2022 paper. The two MD students said they and their fellow researchers had a passion for the work that stemmed from witnessing the impacts of the opioid epidemic firsthand.
“All of us have been touched in one way or another, losing a family member or dear friend or just watching the toll that the opioid epidemic takes on a community,” Haslund-Gourley said. “Seeing the community affected and losing good friends led me to want to get involved and try to not only address people who are suffering, but also attempt to change the way we think about the opioid use disorders as a society.”
“People I grew up with in the Philadelphia suburbs have fallen into using drugs, and some of the kids I grew up playing hockey with have overdosed,” Bascou said. “Opioid use disorder is looked at as a social issue, but it’s also a medical issue, and something we as a society need to treat as a real disease.”

How the study worked
Student researchers surveyed participants before and after a three-hour training on using naloxone to reverse an opioid overdose. The surveys assessed individuals’ attitudes toward naloxone use and overdose reversal, their confidence in their ability to use naloxone or safely help someone experiencing an overdose, and their attitudes toward people with opioid use disorder.
As in previous studies, students found that participants’ knowledge of facts around naloxone and overdose reversal increased, as did participants’ confidence that they could safely help someone experiencing an overdose. Previous studies have also found, as the Drexel and Cooper students’ study did, that participants’ attitudes toward naloxone and overdose reversal improved because of training.
The students’ research expanded on earlier studies by analyzing participants’ attitudes toward those with opioid use disorder before and after training. After the training, participants self-reported having a better understanding of opioid use disorder, seeing beyond stereotypes and preconceived notions.
Study participants included Philadelphia and South Jersey health professionals, health care professions students, medical residents, recovery program providers and members of law enforcement. Because of this, the authors believe the training can be widely applied to help increase overdose reversal success and reduce opioid use disorder stigma.
Students said the content of the training sessions was what helped change participants’ attitudes about opioid use disorder. In addition to teaching participants about opioids, overdose and reversal with naloxone, presentations during the training focused on the societal factors that have created, exacerbated, and prolonged the opioid epidemic, Bascou explained.
“Our training talks about someone living with opioid use disorder, the struggles they feel and what they go through on a daily basis,” Bascou said. “One of the big goals of our training is transitioning potential adversaries or people who are indifferent into advocates or allies.”
Also helpful in achieving that goal are testimonials given during the training by guest speakers who have lived with opioid use disorder.
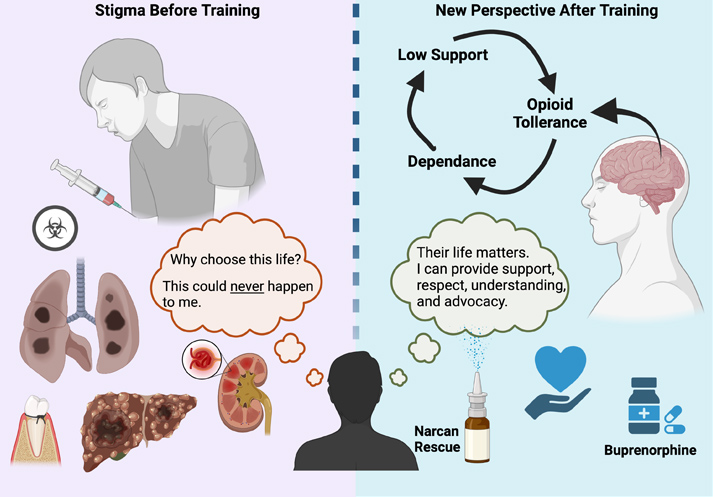
An educational infographic (courtesy of Ben Haslund-Gourley) shows training participants' beliefs about opioid use disorder and people living with before the training and after the training.
“We try to humanize people as much as possible,” Haslund-Gourley said. “Our training is certainly more involved and holistic than simply showing participants: ‘Here’s how to use Narcan.’”
The authors hope that reducing stigma around opioid use disorder will also reduce fear, judgment or rejection for people living with the condition. Less stigma may make it easier for people to seek treatment for opioid use disorder.
Gadegbeku said the awareness-raising students do around the realities of opioid use disorder during the training is crucial.
“I think the training does a great job of going into the history of the opioid crisis, and humanizing people with opioid use disorder,” Gadegbeku said.
What’s next for NOP’s training model?
Current NOP students will work to find out how long the positive effects on participants’ perceptions of those with opioid use disorder last beyond the training session, Haslund-Gourley said.
Gadegbeku will continue to serve as faculty advisor for NOP student researchers, as she has since NOP’s inception in 2017 and for the Drexel students who helped co-author the January 2022 paper.
“I’m really proud of what Ben and his cohort and the prior NOP students have done with this research,” she said. “We hope to carry it forward; it’s really about carrying education and awareness forward.”