Hospitals Helping Violence Victims Could Save Millions
 By Rachel Ewing
By Rachel Ewing
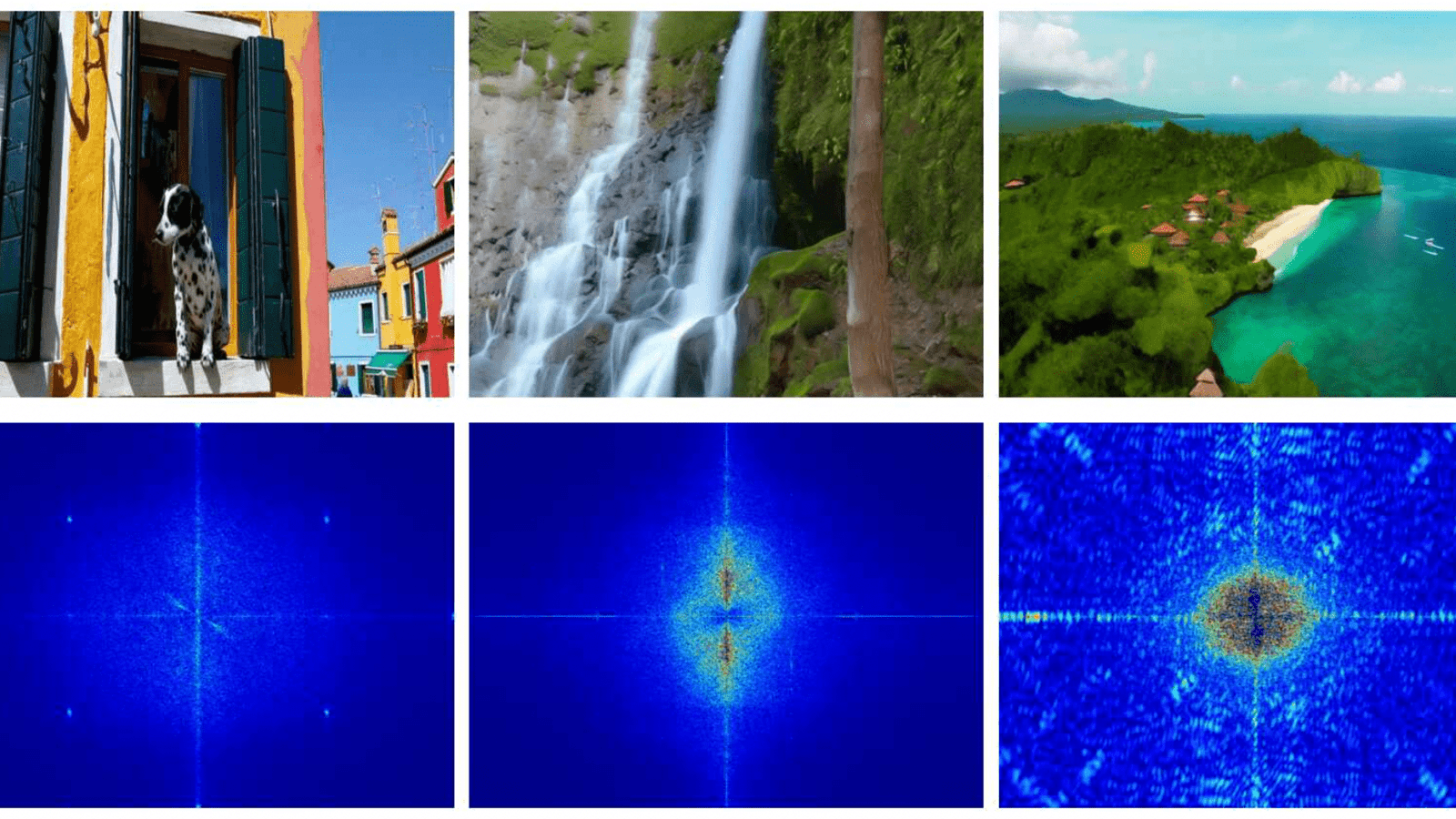
- On the Trail of Deepfakes, Drexel Researchers Identify ‘Fingerprints’ of AI-Generated Video
- New AI-Technology Estimates Brain Age Using Low-Cost EEG Device
- Bolstered by Research Consortium with Drexel, Jefferson’s Sidney Kimmel Cancer Center Earns NCI Comprehensive Cancer Center Designation
- Alyssa Kemp Named as 2024 Truman Scholar

At more than 25 hospitals across the U.S., health care professionals have embraced a public health approach to their work—taking action to prevent violent injuries, not just treat them. In programs known as hospital-based violence intervention programs (HVIPs), teams of medical professionals, social workers and researchers step in at a critical moment in a patient’s life—the period following a violent injury such as a gunshot or stab wound—with case management, counseling and other services that help these victims break free from the cycle of violence.
As these programs have grown, up from about six programs in 2009, reports of their successes have accrued. There is evidence that HVIPs prevent violent reinjury and perpetration, reduce aggressive behaviors and improve employment, education and healthcare utilization among program participants.
Researchers at Drexel University have now published the first study to systematically look at the economic outcomes of hospital-based violence intervention. They demonstrate that, in addition to transforming victims’ lives, these programs may indeed save a significant amount of money compared to non-intervention, in various sectors including health care and criminal justice. They report in the February issue of the American Journal of Preventive Medicine that an HVIP serving 90 clients could result in costs savings from tens of thousands of dollars and up to about $4 million in a five-year period.
“This is the first systematic economic evaluation of a hospital-based violence intervention program, and it’s done in a way that can be replicated as new evidence emerges about the programs’ impacts across different sectors,” said Jonathan Purtle, DrPH, an assistant professor at the Drexel University School of Public Health who was lead author of the simulation study.
Attaching dollars and cents to HVIPs—and knowing which sectors of society are likely to see the financial benefit—is important because many HVIPs lack a sustainable funding source. Most programs currently rely on a patchwork of funders that may include some use of insurance billing for eligible services, such as behavioral counseling; private foundation grant or institutional funding; or local government funding.
Demonstrating that HVIPs are a source of long-term cost savings for the health care system or for the criminal justice system, or both, helps make the case that investing in HVIPs pays off.
Purtle’s study drew on the research literature about violent reinjury, violent perpetration, and estimates of the rates at which HVIPs prevent these outcomes. He compared the costs of outcomes likely to be experienced by a hypothetical group of 90 individuals who received HVIP services (plus the costs of providing HVIP services to the 90 clients, $350,000 per year) to the costs of the outcomes likely to be experienced by a similar group of 90 individuals who did not receive HVIP services. Various models of the simulation included costs to the health care system, such as costs of treating the individuals who are reinjured and/or treating their victims if those individuals go on to perpetrate violence against others; those health care costs plus costs to the criminal justice system to prosecute and incarcerate individuals who become perpetrators; and the preceding costs in addition to societal costs of lost productivity.
In all models of the simulation, HVIPs produced cost savings over five years. The most conservative simulation, including only the future health care costs of those among the 90 individuals who may experience violent reinjury, showed health care savings of $82,765. The most comprehensive model, including lost productivity costs, showed a societal cost savings of over $4 million to serve 90 clients.
Purtle noted that lost productivity costs, while common in economic analyses, may be somewhat unrealistically high because they assume all individuals in the model are employed. Conversely, beyond the economic analysis there are still social benefits of HVIPs that aren’t easily quantifiable: “Even if the intervention cost a little more than it saved in dollars and cents to the health care system, there would still be a net benefit in terms of the violence it prevented,” Purtle said.
A Closer Look: Healing Hurt People in Philadelphia and the Benefits of Hospital-Based Violence Intervention
“The research literature has poetically referred to the time after a traumatic injury as the ‘golden hour’,” said Ted Corbin, MD, an associate professor in Drexel’s College of Medicine and School of Public Health, and a co-author of the study with Purtle. That first hour after a major injury is a medically critical time to address physical symptoms such as blood loss and brain injury.
Soon thereafter, Corbin said, is also a critical, vulnerable moment when patients who were victims of interpersonal violence may direct their thoughts toward retaliation, or toward turning their lives around.
Corbin directs Healing Hurt People, the hospital-based violence intervention program in Philadelphia, based in Drexel’s interdisciplinary Center for Nonviolence and Social Justice, of which he, Purtle and all of the study’s co-authors are part. Healing Hurt People serves a population of pediatric and young adult clients in two inner-city hospitals, who are largely marginalized, underresourced and socially disenfranchised. It operates based on a framework that is trauma-informed—meaning that the program is designed on principles recognizing how traumatic stress and adversity associated with past exposure to violence affect clients and their needs.
“Our efforts are to connect with that person, gain their trust and work to connect them with services,” Corbin said. The majority of patients approached by the program’s caseworkers, either during their time in the hospital or soon after, are interested in enrolling as clients. Many use the assistance of case managers to enroll in health insurance and connect to a primary care doctor for the first time as adults, get an ID card, connect with court advocacy and compensation services for victims, access school services or otherwise pursue positive changes in their lives to avoid future involvement with violence.
The Healing Hurt People program receives financial backing for trauma-informed case management services from the City of Philadelphia’s Department of Behavioral Health and Intellectual disAbility Services. Many of the behavioral health counseling services within the program are billed to insurance when appropriate.
“There are many aspects of society where people can take steps to address trauma and step in to contribute to reducing violence,” Corbin said. “Those of us in medicine have an opportunity to do something through hospital-based violence intervention, but it’s just one slice of the pie.”
Drexel News is produced by
University Marketing and Communications.