Pregnancy is a Missed Opportunity for HIV-Infected Women to Gain Control Over Condition
 By Rachel Ewing
By Rachel Ewing

- Drexel Names Trustee and Area Business Leader Denis P. O'Brien Interim President
- Is Climate Change Keeping Patients from Vital Doctor Appointments?
- Drexel Team Identifies Drug-like Molecules That Show Early Success in Targeting Breast Cancer Brain Metastases
- Mapping the Surfaces of MXenes Atom by Atom Reveals New Potential for the 2D Materials
Pregnancy could be a turning point for HIV-infected women, when they have the opportunity to manage their infection, prevent transmission to their new baby and enter a long-term pattern of maintenance of HIV care after giving birth—but most HIV-infected women aren’t getting that chance. That is the major message from a pair of new studies in Philadelphia, one published early online this month in the journal Clinical Infectious Diseases, and the other published in July in PLOS ONE.
The studies, led by a team of researchers from Drexel University and the Philadelphia Department of Public Health (PDPH), are the first to describe the HIV care continuum postpartum and the first to use population-based data to evaluate viral suppression rates of HIV-infected pregnant women at delivery. Both studies were based on the review of medical records of all HIV-infected women delivering babies in Philadelphia over several years (2005-2011 and 2005-2013, respectively).
In the PLOS ONE paper, the researchers report that women’s engagement in prenatal care was poorer than expected. Only about a third of women received adequate prenatal care, a third received an intermediate level of care, and a third received prenatal care that was inadequate.
At delivery, that care disparity manifested with only about half of women having their HIV viral levels suppressed—an outcome that physicians and public health officials target to prevent transmission of the infection.
“We had expected the viral suppression rate to be much better at delivery because there is a known infrastructure to prevent mother-to-child transmission of HIV,” said Florence Momplaisir, MD, MSHP, an assistant professor at the Drexel University College of Medicine who was lead author of the PLOS ONE study and senior author of the Clinical Infectious Diseases study. Momplaisir also holds an appointment as assistant professor in Drexel's School of Public Health.
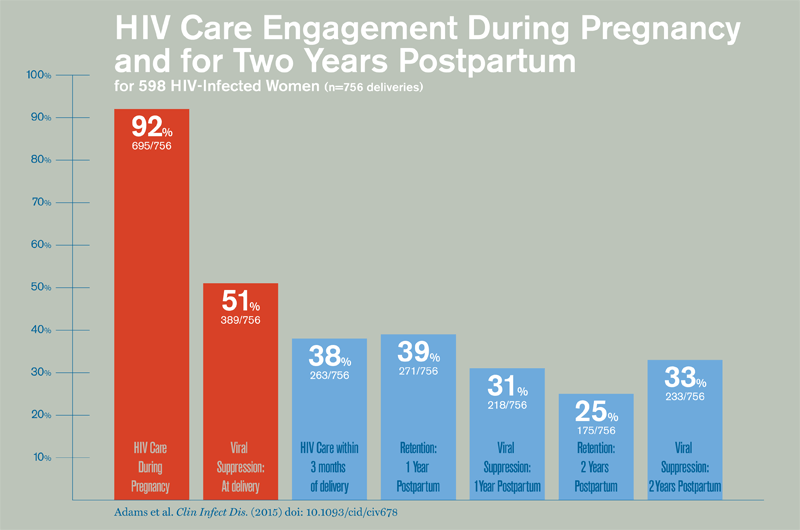
In the latter study, Momplaisir and colleagues took a closer look at the pregnant women’s HIV care during pregnancy and for two years postpartum. They found that HIV care during pregnancy was robust, with 92 percent of women receiving antiretroviral therapy or an HIV lab test during that time. But in the postpartum period, women were far less engaged in HIV care, with only 38 percent of women engaged in care within 90 days after giving birth.
Another major finding: “When women connected with care soon after delivery, they were much more likely to remain in care up to two years afterward,” said Joëlla Adams, MPH, lead author of the Clinical Infectious Diseases study.
Adams, who now works at the Philadelphia Department of Public Health, led much of the data analysis for this study as an MPH student completing a community-based master’s project for the Drexel University School of Public Health at PDPH in 2014. Adams’ project mentors in addition to Momplaisir, Yvonne Michael, ScD, an associate professor at the Drexel University School of Public Health, and Kathleen Brady, MD, MSCE, medical director of the AIDS Activities Coordinating Office of PDPH, were among the co-authors.
“Women engaged in care within 90 days of delivery were 11 times as likely to be retained in care and twice as likely to be virally suppressed at a year postpartum,” said Momplaisir. “This suggests there is a window of opportunity after delivery to establish lasting care.”
The takeaway message, they say, is that HIV-infected women need better interventions and supports to help keep them in care during that critical window, among other times, including before becoming pregnant.
Momplaisir’s continuing studies aim to better understand women’s needs and inform such interventions. She was recently selected as a scholar of the Harold Amos Medical Faculty Development Program of the Robert Wood Johnson Foundation to understand how personal factors including women's social norms, perceived beliefs, social support and personal barriers such as untreated mental health, substance abuse, intimate partner violence, and health system factors, including whether women receive HIV and obstetric care together or separately, contribute to HIV outcomes. In addition, she received an Early Career Investigator Award from the International Maternal Pediatric Adolescent AIDS Clinical Trial Network (IMPAACT) to use data from an existing IMPAACT trial to understand how depression affects the quality of HIV care that pregnant and postpartum women receive.
“Although we have made enormous achievements in reducing mother-to-child transmission of HIV in the U.S., there is more work to be done to completely eliminate that risk and to ensure that HIV-infected women of child bearing age are living healthy and productive lives,” Momplaisir said.
Drexel News is produced by
University Marketing and Communications.