Racial and Ethnic Health Disparities Persist for Individuals with Autism
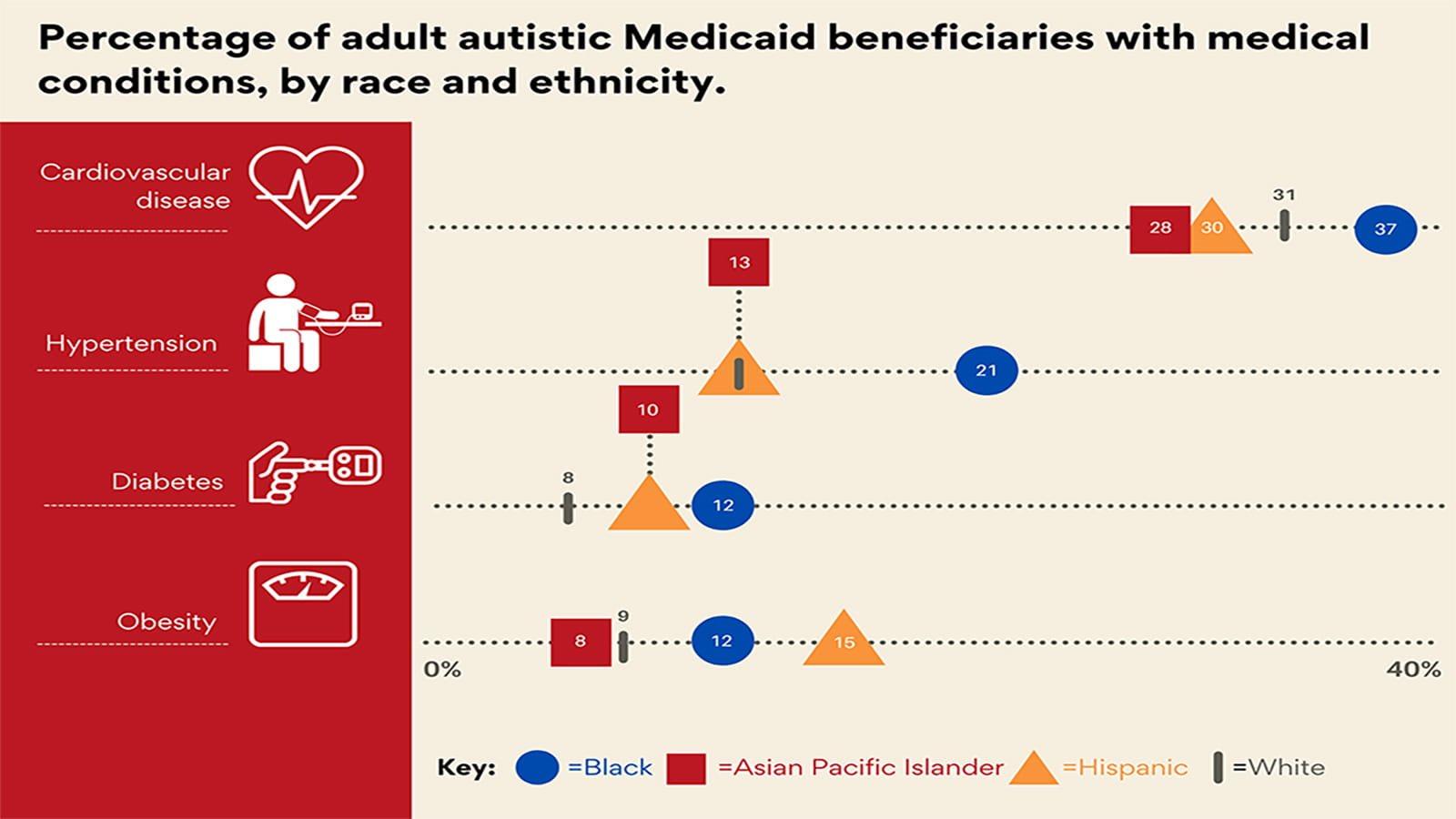
Using Medicaid data, researchers from the A.J. Drexel Autism Institute identified health conditions that varied in prevalence. They found a higher prevalence of heart disease, hypertension, diabetes and obesity by race. Image credit: A.J. Drexel Autism Institute
Often autistic adults can have several co-occurring physical and mental health conditions and, like in non-autistic adults, these may differ by racial and/or ethnic group. Researchers from Drexel University’s A.J. Drexel Autism Institute recently published research showing autistic adults on Medicaid have increased odds of some health, nutrition and psychiatric conditions, compared to the general Medicaid population.
The research also showed that many of the same health disparities by racial/ethnic group in the general population persist among the autistic adult Medicaid population. For example, Black, Hispanic and Asian autistic adults on Medicaid have higher odds of diabetes, and Black and Hispanic autistic adults have higher odds of obesity and nutrition conditions, compared to white autistic adults on Medicaid.
The research team examined Medicaid claims data from 2008–2012 to examine adults ages 18-64, including the full population of adults with autism and created a comparison group from a random sample of beneficiaries without an autism diagnosis. They identified prevalence of co-occurring physical and mental health conditions for these groups and were able to estimate the association of autism diagnosis with those conditions. Finally, using only the population with an autism diagnosis, they estimated the association of racial/ethnic category with each physical and mental health diagnosis.
These findings suggest that, as a whole, autistic adults on Medicaid are not at higher risk of certain severe physical health conditions, such as stroke and cardiovascular disease compared to other Medicaid beneficiaries. However, they are at higher risk of some important health conditions – including conditions such as epilepsy, seizures, Parkinson’s disease and nutrition conditions. Moreover, researchers found important racial disparities in physical health conditions, with Black, Hispanic and Asian autistic adults on Medicaid having higher odds of conditions like diabetes, hypertension and stroke.
“We need to consider ways to reach families with autistic members to ensure they receive preventive health measures and screenings for these conditions,” said Whitney Schott, PhD, a research scientist at the Autism Institute and lead author on the study. “For example, clinicians and public health programs can reach out to patients and families with public health messages and reminders or explore ways of communicating more frequently with patients.”
Autistic adults enrolled in Medicaid have higher odds of mental health diagnoses, including anxiety disorder, attention deficit hyperactivity disorder (ADHD), bipolar and obsessive-compulsive disorder, compared to the general Medicaid population. However, analysis by racial/ethnic group suggests that these diagnoses are less common among Asian, Black and Hispanic autistic adults on Medicaid.
“New and different strategies to ensure access to preventive care, screening and regular monitoring are needed to address health inequities among autistic adults,” said Lindsay Shea, DrPH, director of the Policy and Analytics Center and interim leader of the Life Course Outcomes Research Program at the Autism Institute, an associate professor and co-author of the report. “We need to support autistic individuals, their families, and clinicians to understand and address the needs of Asian, Black and Hispanic groups within Medicaid since it is an important insurer across the lifespan.”
The researchers explained it is important to examine whether the lower odds of diagnosis with various mental health conditions among Asian, Black and Hispanic beneficiaries is a true difference, or whether there is a lack of access to diagnostic and mental health services for these groups.
“The call to action to address health inequities across groups of autistic adults is urgent since the care they need cannot and should not wait. We need medical and public health solutions to engage these groups directly and work together to create change in how they can access the health care they need all along the way,” said Shea. “We should not be waiting until a person has a serious medical condition to serve them. We have opportunities to deliver preventive care that can improve health and well-being now, but we must restructure our approaches to make it a reality.”
The study, “Co-Occurring Conditions and Racial-Ethnic Disparities: Medicaid Enrolled Adults on the Autism Spectrum," was recently published in Autism Research.
Drexel News is produced by
University Marketing and Communications.
