Power Over Pain
November 30, 2017
 According to the Institute of Medicine, chronic pain is a major health issue affecting approximately 100 million Americans and amounting to a cost of roughly $635 million a year. The healthcare community has a history of poor outcomes for chronic pain that have frustrated both patients and providers. Chronic pain can be very challenging to treat. It is an evolving condition with remodeling of neurological structures and biological, behavioral, environmental and societal influences. The focus is shifting from eliminating pain completely to minimizing the impact of pain on quality of life and building resilience to better cope with chronicity. The opioid crisis has drawn attention to how chronic pain is understood and managed. In 2016, the Centers for Disease Control and Prevention recommended that nonpharmacological therapies be the first line treatment of chronic pain. Mental health, physical therapy and a variety of other professions and wellness strategies are fast becoming that first line defense. Interdisciplinary approaches are considered best practice in treating both chronic pain and substance use disorders. Interdisciplinary care that addresses health and wellness across physical, mental, and social domains is most effective. Healthcare providers need to have a good understanding of chronic pain neuroscience, biopsychosocial components of pain management, issues related to substance use disorders and pain management strategies so that they can effectively integrate their expertise within the context of interdisciplinary care and reinforce strategies used by other team members.
According to the Institute of Medicine, chronic pain is a major health issue affecting approximately 100 million Americans and amounting to a cost of roughly $635 million a year. The healthcare community has a history of poor outcomes for chronic pain that have frustrated both patients and providers. Chronic pain can be very challenging to treat. It is an evolving condition with remodeling of neurological structures and biological, behavioral, environmental and societal influences. The focus is shifting from eliminating pain completely to minimizing the impact of pain on quality of life and building resilience to better cope with chronicity. The opioid crisis has drawn attention to how chronic pain is understood and managed. In 2016, the Centers for Disease Control and Prevention recommended that nonpharmacological therapies be the first line treatment of chronic pain. Mental health, physical therapy and a variety of other professions and wellness strategies are fast becoming that first line defense. Interdisciplinary approaches are considered best practice in treating both chronic pain and substance use disorders. Interdisciplinary care that addresses health and wellness across physical, mental, and social domains is most effective. Healthcare providers need to have a good understanding of chronic pain neuroscience, biopsychosocial components of pain management, issues related to substance use disorders and pain management strategies so that they can effectively integrate their expertise within the context of interdisciplinary care and reinforce strategies used by other team members.
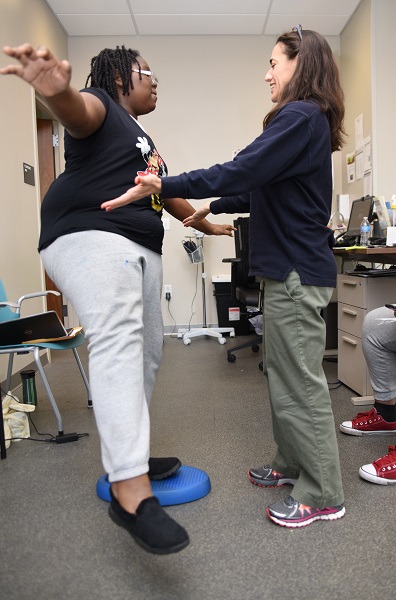
 At Drexel University’s Stephen and Sandra Sheller 11th Street Family Health Services, we developed a psychoeducational group called Power Over Pain (PoP). Research has indicated that an interdisciplinary approach aids in improving the functional status and quality of life of patients with chronic pain. PoP is an interdisciplinary program that empowers patients through education to self-manage their pain. The group is based on a framework we developed, the Clinical Reasoning Model for Chronic Pain.
At Drexel University’s Stephen and Sandra Sheller 11th Street Family Health Services, we developed a psychoeducational group called Power Over Pain (PoP). Research has indicated that an interdisciplinary approach aids in improving the functional status and quality of life of patients with chronic pain. PoP is an interdisciplinary program that empowers patients through education to self-manage their pain. The group is based on a framework we developed, the Clinical Reasoning Model for Chronic Pain.

The top of the diagram represents the goal of treatment: patients who are using healthcare services appropriately as they self-manage their pain with little or no opioid use. To reach this goal, patients need education, mentorship for behavioral change, help to address cognitive-affective factors and an understanding of the roles various healthcare providers serve in their health and wellness.
 The middle of the diagram depicts an interdisciplinary team that includes the patient. All members of the interdisciplinary team collaborate to arrive at unified goals and a unified plan of care. This differs from a multidisciplinary approach where patients see different professionals who are not functioning as a cohesive team, each providing different goals and treatment plans leaving the patient to sort through an often overwhelming amount of information and action items. Good communication among professionals, the patient, the patient’s family and other stakeholders is essential in forming the collaboration needed for efficient and effective care management.
The middle of the diagram depicts an interdisciplinary team that includes the patient. All members of the interdisciplinary team collaborate to arrive at unified goals and a unified plan of care. This differs from a multidisciplinary approach where patients see different professionals who are not functioning as a cohesive team, each providing different goals and treatment plans leaving the patient to sort through an often overwhelming amount of information and action items. Good communication among professionals, the patient, the patient’s family and other stakeholders is essential in forming the collaboration needed for efficient and effective care management.
Each pillar at the bottom of the model represents a different area of research important for chronic pain management. While each team member specializes in their discipline, everyone should have a broad knowledge of all areas so that they can effectively situate their expertise within the fabric of the whole patient and a holistic treatment approach that will prepare patients for a resilient path forward.
The PoP group will be re-starting at Stephen and Sandra Sheller 11th Street Family Health Services and will be offered for the first time at Parkway Health and Wellness in this spring. Information about the group and its curriculum can be found at http://poweroverpain.sarah.pt/.
*Note: Wenger's article, “Reducing Opioid Use for Patients with Chronic Pain: An Evidence Based Perspective,” is getting published in the Physical Therapy Journal in print in April and on-line early 2018.
By Sarah Wenger, PT, DPT, OCS
Associate Clinical Professor, Coordinator of Experiential Learning
Physical Therapy and Rehabilitation Sciences Department