Stroke Risk Factors Centered in Southeast United States
 By Frank Otto
By Frank Otto

- Drexel Environmental Collaboratory Releases Cross-Sector Findings on Severe Weather Recovery Challenges
- Drexel Launches the Manuel Stamatakis Center for Alternative Investments at the LeBow College of Business
- How and When Could AI Be Used in Emergency Medicine?
- Faculty Highlights: Recent Awards and Grants
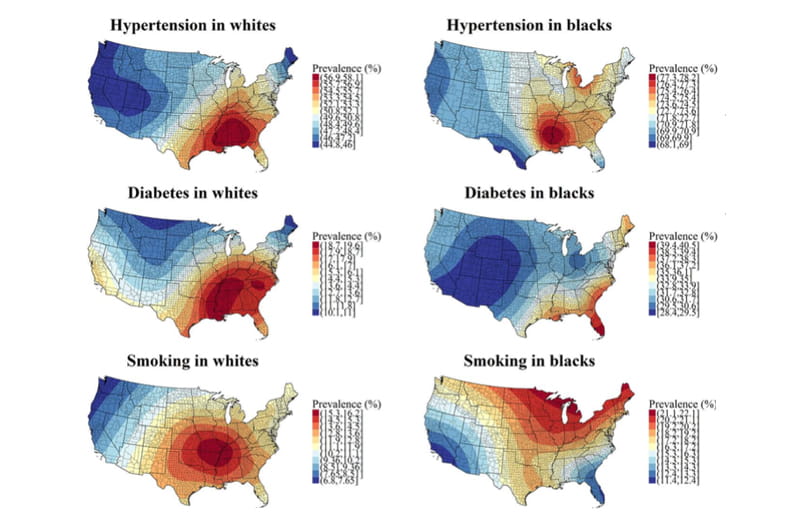
The Southeastern United States features the highest concentrations of people living with stroke risk factors like high blood pressure, diabetes and smoking, according to researchers who mapped the data.
“Our findings show that the geographic distribution of stroke risk factors mirrors the geographic distribution of stroke mortality, which suggests that higher prevalence of risk factors in certain areas may be associated with higher risk of outcomes,” said Leslie McClure, PhD, a professor in Drexel University’s Dornsife School of Public Health, who served as senior author on the study. “Trying to understand why is the next step in this analysis.”
A former student of McClure’s, Mathew Loop, PhD, now an assistant professor at the University of North Carolina, led the study, published in Circulation: Cardiovascular Quality and Outcomes. Their team intended to map the prevalence of hypertension (high blood pressure), diabetes and smoking — all considered major risk factors for stroke — across the United States.
By using data collected from participants between 2003 and 2007 for the National Institutes of Health’s Reasons for Geographic and Racial Differences in Stroke (REGARDS) population health study, the researchers hoped to get a good idea of the distribution of risk factors. Participants in the study were 45 years of age or older, and the data was sorted into white and black participants to determine if there were any racial disparities in the geographic distribution of the prevalence of certain risk factors.
“Understanding the geographic distributions of risk factors is important to understanding where to focus clinical interventions and policy changes so that they can be most effective,” McClure explained.
Data showed that the population of the Southeastern United States exhibited the highest prevalence of most risk factors, especially among white participants. In fact, all three of the measured risk factors had their highest prevalence in the Southeast when it came to white people — though the epicenter of whites who smoke actually shifted toward the Midwest.
Hypertension in black participants was highest in the Southeast as well, though its epicenter was also shifted, this time slightly further west toward the borders of Mississippi, Louisiana and Arkansas (hypertension among whites was centered on Alabama and spilled into Mississippi, Georgia, the Florida Panhandle and the lower portions of Tennessee).
There were much clearer differences in the distribution of diabetes and smoking among black participants.
The highest prevalence of diabetes in black participants was centered in southern Florida, with elevated prevalence extending along the southern coast of the Atlantic and the coast of the Gulf of Mexico.
Smoking among black participants was highest in the northern Midwest, with Michigan, Wisconsin and Minnesota’s northern points showing the highest rates.
Overall, though, black participants exhibited higher rates of risk factors than whites, with 71% of black participants having hypertension compared to 51% of whites. A similar disparity existed in diabetes (31 percent in blacks to 16 percent in whites) and in smoking (17 to 13 percent, respectively).
“It’s important to keep in mind that there are several things that may contribute to different racial patterns in risk factors that we haven’t considered in this study, such as socioeconomic factors,” McClure said. “That being said, the difference in racial distributions is important for the purpose of targeting policies and making clinical changes.”
Regardless of race, many of the findings fell along what’s been dubbed the “Stroke Belt.” The Belt extends through Arkansas, Louisiana, Mississippi, Alabama, Tennessee, Georgia, South Carolina and North Carolina, where past research has shown elevated incidences of strokes. The researchers hope the knowledge of the correlated locations between stroke and risk factor can provide a leg up on prevention.
“If we can minimize the prevalence of risk factors, then this should help reduce the incidence of disease,” McClure said. “Understanding the areas of the country that have these factors, then, is important for targeting effective interventions.”
Those interested in the full study can access it here: “Heat Maps of Hypertension, Diabetes Mellitus, and Smoking in the Continental United States.”
In This Article
Contact
Drexel News is produced by
University Marketing and Communications.