Q&A: Indoor Masking and Understanding Where We Are in the COVID-19 Pandemic

Please visit the ‘Drexel’s Response to Coronavirus’ website for the latest public health guidance.
On April 11, Philadelphia announced the reinstatement of an indoor mask mandate starting April 18, in response to a new level of increasing COVID-19 cases and hospitalizations in the city. The change to Level 2, based on Philadelphia COVID case data metrics, is aimed at stemming the rise in cases related to the highly transmissible Omicron BA.2 subvariant that is in our region.
Drexel University, as announced in an April 14 message from its Return Oversight Committee (ROC), will move to indoor masking in accordance with the city’s mandate. Starting April 18, masks are required in most indoor spaces on campus. Previously, the University was following a two-tiered masking system in which some Drexel campus spaces (including classrooms while class is in session) required masks, while others were “masks optional” areas.
In this Q&A, Chief Wellness Officer and Senior Vice Provost for Community Health Marla Gold, MD, explained why this preventative move was made and what it means for both Drexel and the city of Philadelphia.
Q: Can you talk about where Drexel is now with the pandemic?
A: At Drexel, we have a highly vaccinated and boosted population with access to testing and contact tracing, and the ventilation has been reviewed on campus. The University community has been doing remarkably well at this point in the pandemic. I say that humbly, knowing that for all of us, COVID can change our collective narrative in unexpected ways.
Upon return after spring break last month, the number of COVID-19 infections among employees (faculty and professional staff) and students was remarkably low for those that were tested. There’s been a slight uptick in the ensuing weeks since the return, similar to the city at large, and we have an eye on that. Our cases from Drexel’s PCR testing program are used to inform our COVID-19 dashboard, but there also are anywhere from two to four other individuals, often employees, who call in every one to two days with COVID infections that they’ve diagnosed at home with a rapid antigen at-home test. Since we cannot reliably collect rapid test data (we would need all the negative rapid tests too!), we don’t include it on our Drexel test data dashboard. In the past week however, cases diagnosed through our three testing sites increased markedly, reflecting the arrival of BA.2 and showing us just how contagious it is. Infections mainly stem from unmasked, social gatherings and exposures at home.
Q: What has Drexel been seeing in terms of trends of infection?
A: The Omicron BA.2 subvariant transmission is high enough and new enough that our community is getting affected by it. We’ve remained masked in the classroom to prevent classroom transmission, noting people can be infectious while asymptomatic and that contact tracing from classroom exposures can be quite disruptive. It’s also a time of year when other respiratory infections are occurring along with seasonal allergies, so masking in classrooms remains important rather than losing class time sorting out illness. We’ve never had classroom transmission while masked. That said, it's our hope that once infections decrease again, there will be a time when masking becomes optional everywhere — we just aren’t there yet.
For the Drexel community, we have closely monitored infections for two years, ensuring excellent care, timely isolation and clear guidelines for those infected and exposed. Infection has not been coming from walking down the hall or working out at the Rec Center. For employees, infections are most typically coming from exposures at home, usually through an infected child, whether that be a young adult or younger child, or a spouse or partner who somehow gets infected, usually from being at an event. For students, infection mostly comes from large social gatherings such as parties, indoor concerts, and bars. These are places where people are in close quarters unmasked, often with large numbers of people that they do not know.
We often talk about Omicron being a “mild” disease and for many, it is. But while we don’t have people routinely needing a hospital or doctor at their bedside, we have plenty of people who experience fever, congestion, muscle aches, painful sore throat, headache and cough. A few have GI symptoms and fewer complain of shortness of breath. As I said, we call it “mild” because hospitalization among a vaccinated community is rare — but people can feel ill, often for 5–7 days. Older individuals may take even longer to feel rested enough to return to work. That said, we have come a long way from the early months of this disease in 2020, when we didn’t have vaccines or good treatment and essentially had no idea what we were dealing with. Overall, things are so much better now.
Q: Can you talk about why it’s important for Drexel to follow Philly’s indoor masking requirements?
A: We must follow city public health guidance — it’s not optional. We believe in prevention and support the city in its efforts to slow transmission. We are part of Philadelphia. Many of us live here; others come here to work and go to school. What happens in Philadelphia affects us, and what happens at Drexel affects Philadelphia. That’s been true and highlighted by the pandemic. We can contribute to a pandemic unwittingly and we can catch disease when viral transmission rises in the city. When disease goes down in the city, we all benefit. A major line of defense to interrupt transmission in our city now is the face mask. A well-fitted, high-grade filter face mask, such as a KF94, KN95 or N95, reduces the risk of infection and transmission while enabling us to go about our day. It is certainly not easy for everyone to do — but masks are best thought of as a way to interrupt transmission and get things to a better place for us all.
Q: What will be happening at Drexel?
A: Starting April 18, in accordance with the city, Drexel will reinstitute masking in many shared spaces on campus. There will be signage on the doors to our libraries and academic and administrative buildings noting masks are required there. Masks were already required in the classroom.
There are some things that are different this time. Masks will remain optional in the Rec Center, and there’ll be signage up about that. We have never had data pointing us to the Rec Center as a source of transmission, nor have we ever had a transmission case in the Rec Center during periods of optional masking. So we’re going to stay optional in the Rec Center. We also think that’s good for mental health when people go to work out, have access to gym equipment and can choose to do that without masking. Masking will also remain optional in Student Residential Housing because that’s where students live — just like masking is optional in employee homes.
Q: So it’s a change in indoor masking, but no shutdowns, right?
A: I know this week when people heard about the return to indoor masking, a lot of them felt like, “Here we go again.” Right away, they felt this is a total shutdown of the city. It’s not. It’s not a total shutdown of the University either. Not even close.
I’m getting questions about food and events. We ask that people stay masked until they’re seated with their food, but events will continue. We’re still allowing events with protocols in place. If the cases go up higher, and the city gives further directives, then Drexel will respond accordingly. If we see disease happening from any of the things that we’re allowing, we’ll reassess. We make these decisions with the realities of people’s everyday lives in mind. Everything we do for COVID-19 combines what the science tells us with what humans tell us and where we are in the pandemic — and then we do our best to enact the least restrictive policies we can.
Q: What would you like people to understand about why this decision is being made?
A: As frustrating as it can seem, the job of public health is to make sure that a small increase in cases doesn’t go any higher. Public health, and I include myself in public health, doesn’t wait for large numbers of people to be in the hospital, because by that time it’s too late. Public health doesn’t wait until there’s a sharp, steep increase in a line — we begin to act sooner, trying to balance prevention measures with peoples’ need to be able to follow the measures and live their lives.
The difficulty for public health is that if we mask up when the numbers are rising but still low overall, and the numbers stay low, people will think we shouldn’t have done anything, and that we were wrong. But if we don’t say anything and the numbers keep rising, and then it’s one of us or someone we love who gets severe COVID, then people will blame public health for not telling them to mask up. People may perceive us as failing no matter what we say about masking, and we would rather have them not get sick. If you gave me a choice, I’d rather have you not get sick.
I realize, for some people, a mask is difficult to wear. I don’t mean to say that it’s not. But for the vast majority, masking is not hard. Masking is understood to be a tool to enable us to continue during this time — and, along the way, perhaps avoid other respiratory diseases and the pollen causing allergies this time of year.
Q: What would you say to those who feel that because they’re vaccinated and Omicron is supposed to milder, getting COVID wouldn’t be that bad?
A: I know that some people feel that this version of Omicron is a milder disease, like a bad head cold, so why are we making people wear masks and isolate just because of a bad head cold? First, it isn’t a bad head cold for everybody. Second, right now we have even young people who don’t feel very well for five to seven days and get bad sore throats, muscle aches, headaches and congestion. Third, we do not know the long-term effects of this disease yet. We feel pretty good that vaccines really help mitigate the risk of long COVID-19, but some people who had COVID have had complications for many months or longer after disease.
We don’t want people to just get COVID and “get it over with.” We don’t want people taking uninformed risks and getting sick. But we recognize that we’re closer than ever to this being a manageable disease, meaning that we know when to mask up and can recognize a high-risk situation and act accordingly. Manageable means that we manage ourselves in a way that is sensible for us as individuals and for us as a population, as a community.
There’s more nuance here in risk assessment and decision-making than there’s ever been before. The fact is that young adults most often have some of the mildest disease with Omicron, compared to older adults, particularly those over 55. But young adults have some of the highest risk behaviors to get COVID. At Drexel, we’re trying to address that — always without being too restrictive or punitive — the best we can by working with Philadelphia’s Department of Public Health and looking at the data.
Q: How should people be navigating masking on campus?
A: Outdoors is always better than indoors. It’s always safer to be outside during increases in COVID variants. It’s better if indoor events can open a door or have a terrace outside. And when indoors, wear a high-grade filtration mask, also known as a respirator, like a KN95 and/or KF94, or certainly N95s if people want to wear them. Those are the best protection for what is a very highly contagious variant. We have a stock of KN95s and KF94s when people forget theirs or can’t access one, and you can find where those are located in the April 14 message.
Q: Anything else you’d like to say?
A: I’ve heard a lot of people want COVID-19 to be “endemic.” Endemic essentially means that we are at the point with a disease where we “accept” a certain amount of disease and death, just like there are other diseases and conditions that cause a certain amount of disease and death. Contrary to what many think, we’re not yet at the point where this disease is endemic in our country or globally. The level of disease is not comparable to flu and other respiratory diseases for what it causes.
Are we closer to endemicity than we’ve ever been before? Absolutely. It’s hard, I know, to avoid discouragement when you hear that masks are back, but there may still be times when we collectively follow enhanced prevention measures during this pandemic. This time with BA.2, many of us hope that hospitalizations remain low in our city, showing an “uncoupling” of severe disease from an increase in cases overall. If that happens, we should expect the city to reconsider its metrics and measures. Meanwhile, we can get to the other side of this increase, hopefully within a few weeks, and we’ll keep moving forward. I hope this blip does not interrupt the flow of our events and our plans. We’ve communicated much to date, to help people understand what they need to do in order to get through this together and still learn, live, be able to socialize and have fun.
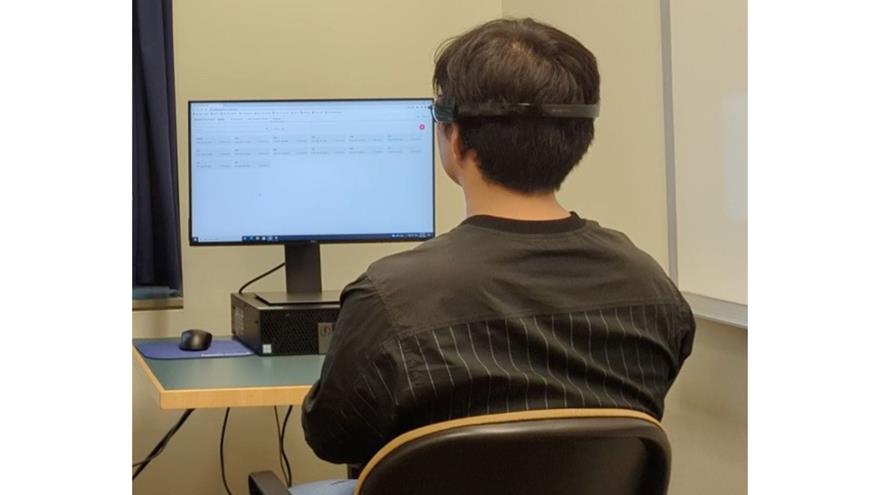
- New AI-Technology Estimates Brain Age Using Low-Cost EEG Device
- Bolstered by Research Consortium with Drexel, Jefferson’s Sidney Kimmel Cancer Center Earns NCI Comprehensive Cancer Center Designation
- Drexel’s Pearlstein Gallery Offers Spring Exhibitions Centered on the Healing Properties of Art and Creative Works
- Pinging Pipes Could Help to Identify Lead Water Lines Without Excavation
In This Article
Drexel News is produced by
University Marketing and Communications.
