The College of Medicine partners with many community organizations to help improve the health and well-being of people in the Philadelphia area and beyond. Our civic-minded approach to learning and our emphasis on real-life problem solving is at the core of a Drexel education. Our students and faculty volunteer countless hours to address health issues by working at local clinics, managing educational programs and running outreach projects, while leveraging university technology and resources. Students also demonstrate service leadership and collaborate with local agencies to support and augment their outreach and success.
From free, student-run health clinics to volunteer opportunities at Philadelphia public schools, our faculty and students take an active role in several community outreach projects. Learn more.
The College of Medicine offers several educational programs for high school students, returning physicians and women in academic medicine. Learn more.
Our work in the community extends beyond the city of Philadelphia. Each year, several medical students participate in international rotations designed to address global health issues. Learn more.
The Institute for Women's Health and Leadership carries forward the College of Medicine's historic commitment to women's health and women's leadership in medicine and science. Learn more.
Upcoming Events
Jun 8
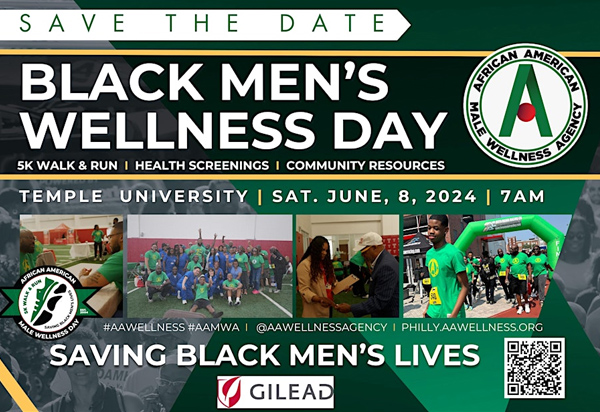
AAWMA Black Men’s Wellness Day
7 a.m. – 12 p.m. (noon)
Temple University
Volunteer Sign Up
Sep 10-21
Community Health, Arts, and the Environment in Cuba for Drexel Students
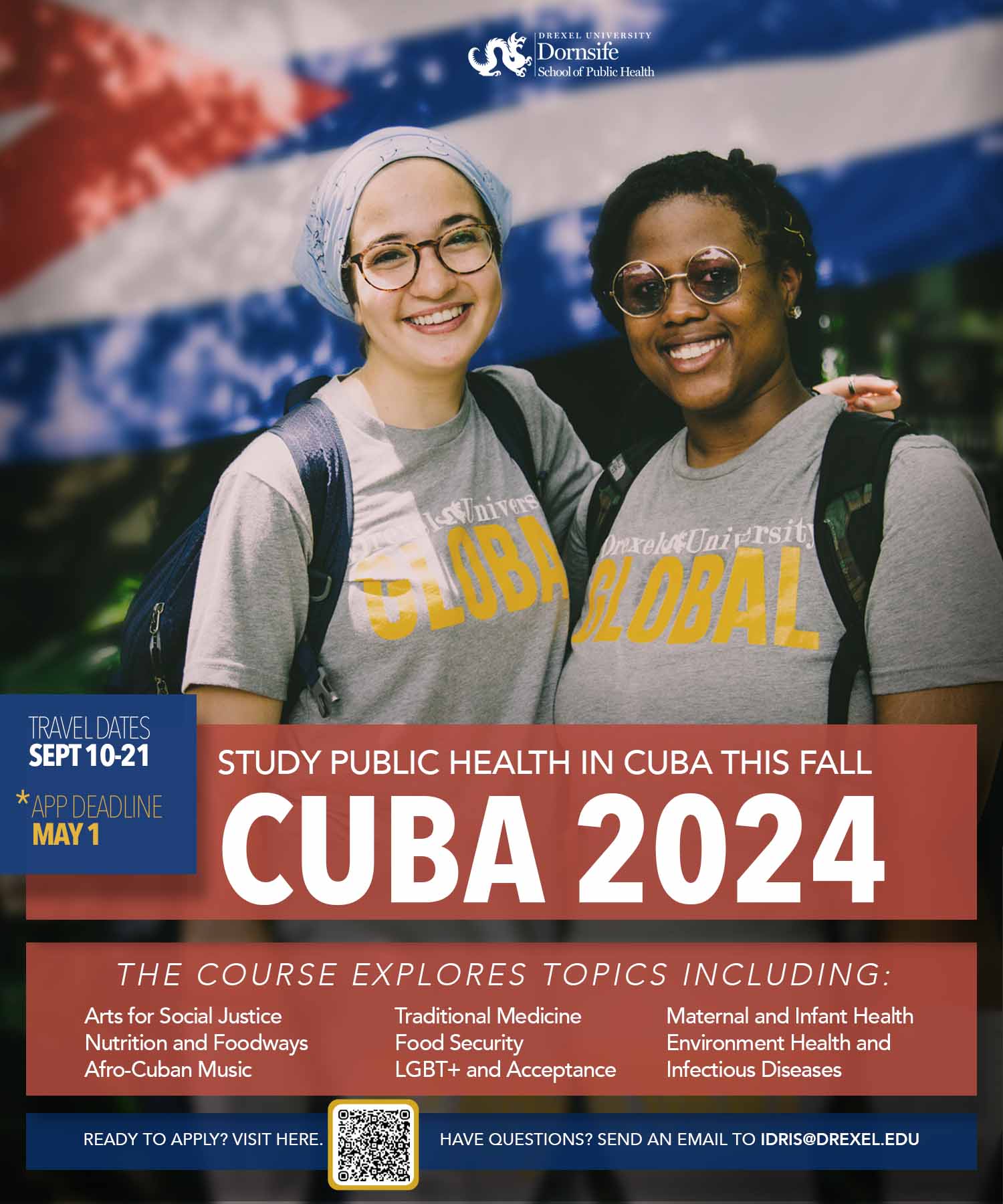
Application Deadline: May 1, 2024
Travel Dates: September 10-21, 2024
Course Facilitators: Joe Amon, Idris Robinson, Nancy Epstein
The application for the CHPT580/CHPT380 Community Health, Arts, and the Environment in Cuba (Cuba CHE) course is now open. Cuba CHE is a 3-credit, fall term Intensive Course Abroad (ICA) that delves into global health concepts through the unique perspective of Cuba. The course is open to all graduate students across the university and upper-class undergraduates. In close collaboration with our partners at the University of Cienfuegos, we will examine how community health, art, and environmental factors influence Cuba's public health system and overall health outcomes. This immersive experience takes Drexel students beyond the classroom and into the resilient communities of scholar activists, community organizers, history preservers, and empowerment artists. Notably, this opportunity is provided with full English translation!
Ready to apply and want to learn more? Visit https://studyabroad.drexel.edu/index.cfm?FuseAction=Programs.ViewProgram&Program_ID=47751.
Have questions? Feel free to contact Idris Robinson (itr24@drexel.edu).
News
The OCHHE Newsletter: Year in Review Edition
See what we have been up to in 2023 and how YOU can get involved in 2024!
SLAMS Program Brings Together Health Professions Community and West Philly Neighbors
Middle school students can be a tough crowd to impress, but Drexel University College of Medicine community members leading educational courses at Science Leadership Academy Middle School (SLAMS) said the students are excited and engaged. Read more.
10th Annual Reach Out and Read Tournament
A recent Philadelphia Tribune story covered the 10th annual Reach Out and Read Tournament, which benefits pediatric literacy programming at St. Christopher's Hospital for Children. Numerous College of Medicine community members participated in the fundraiser, which this year raised over $150,000. Medical students and faculty members from Drexel collaborated with local medical residents to offer health screenings and information during the event. The Office of Diversity, Equity and Inclusion also sponsored the College of Medicine’s student basketball team, which competed in the tournament. Read more.
Fighting Addiction Stigma
Students at the College of Medicine are destigmatizing opioid use disorder to improve overdose reversal training and advocate for new treatments. Exel - Drexel University Research Magazine (2023)
HOP Broadens Reach in Berks County
While the Health Outreach Project (HOP) has been part of the College of Medicine’s culture for more than 25 years, the programming only expanded to Berks County, Pennsylvania, in 2021, when the College of Medicine at Tower Health opened in West Reading. HOP faculty advisor Eugene York, MD, is impressed with the work students have done to grow HOP programming around the campus. “It has been amazing, in a little over a year, to see what they have started and what they’ve accomplished so far,” York says. Read more.
Back to Top